The Rise of Allergies and Autoimmune Diseases: What’s Behind the Epidemic?
Introduction
In recent years, allergies and autoimmune diseases have become an increasingly common health concern. From mild skin reactions to life-threatening conditions like peanut allergies, these diseases impact millions of people globally. The question is: why are modern humans more susceptible to these immune system disorders than our ancestors? In his book An Epidemic of Absence: A New Way of Understanding Allergies and Autoimmune Diseases, science writer Moises Velasquez-Manoff delves into this critical question, explaining how our modern environment—particularly our reduced exposure to microbes—has played a key role in the rise of these diseases. This article explores Velasquez-Manoff’s research, providing insights into the functioning of the immune system, the relationship between allergies and autoimmune diseases, and the potential new treatments that might offer relief.
Understanding the Immune System and How It Protects Us
The immune system serves as our body’s defense mechanism against harmful substances, infections, and disease. It operates in two main ways: preventing harmful agents from entering the body and eliminating harmful cells inside the body.
First Line of Defense:
The first line of defense includes our skin and mucous membranes. These physical barriers block pathogens from entering the body. For instance, sweat helps flush away foreign particles, and tears contain lysozymes that break down bacterial cell walls.
Second Line of Defense:
The second line involves cells like phagocytes and enzymes that actively fight infections. When a foreign substance breaches the outer defenses, phagocytes (specialized immune cells) detect and engulf the invader to prevent it from spreading.
Third Line of Defense:
The third line is made up of immune organs like the thymus, spleen, and lymph nodes, where lymphocytes (white blood cells) serve as the elite defenders. These cells can also “remember” previous invaders, making future immune responses faster and more effective.
Allergies: When the Immune System Overreacts
What Are Allergies?
An allergy is a reaction by the immune system to a substance that is usually harmless to most people. When someone with an allergy comes into contact with a trigger (like pollen or peanuts), their immune system mistakenly identifies it as a threat and overreacts. This can lead to symptoms like hives, wheezing, rashes, or in severe cases, anaphylaxis.
Types of Allergies:
- Food Allergies: A common example is peanut allergies, where the immune system mistakenly identifies peanut proteins as harmful, triggering severe reactions. The rates of peanut allergies have increased significantly in recent decades.
- Respiratory Allergies: Conditions like asthma are common, where the immune system overreacts to airborne allergens like dust, pollen, or pet dander.
- Skin Allergies: Conditions like eczema or allergic dermatitis occur when the skin becomes overly sensitive to substances it would normally tolerate.
Autoimmune Diseases: When the Immune System Attacks Itself
Autoimmune diseases occur when the immune system mistakenly targets the body’s own tissues as foreign invaders, leading to chronic inflammation and damage. Some well-known autoimmune diseases include:
- Rheumatoid Arthritis (RA): The immune system attacks the joints, causing pain, swelling, and potential joint damage.
- Systemic Lupus Erythematosus (SLE): In this condition, the immune system attacks connective tissues throughout the body, which can affect organs like the kidneys, heart, and lungs.
- Multiple Sclerosis (MS): The immune system attacks the central nervous system, leading to symptoms like muscle weakness, numbness, and difficulty with coordination.
The Role of Microbes in Our Health: The Missing Link
Microbes and Immune Development:
Humans have evolved in environments teeming with microbes—bacteria, viruses, fungi, and parasites. Our immune system co-evolved with these microbes, learning to distinguish between harmful and benign agents. However, with modern hygiene, medicine, and lifestyle changes, many people are exposed to far fewer microbes than our ancestors.
This lack of microbial exposure is believed to be a major contributing factor to the rise in allergies and autoimmune diseases. The hygiene hypothesis suggests that reduced exposure to microbes during childhood can lead to an underdeveloped immune system, which overreacts to harmless substances.
Historical Microbial Exposure:
- Ancient Exposure: For centuries, humans lived in environments filled with parasites and infections. Archaeological evidence shows that ancient Egyptians and Romans had parasitic infections, while the Industrial Revolution in the 19th century saw urban populations living in close proximity to pathogens, leading to widespread diseases like tuberculosis.
- Modern Cleanliness: Since the discovery of antibiotics and improvements in sanitation, many of these dangerous pathogens have been controlled. But as a result, our immune systems are no longer “trained” by these microbes, which may lead to immune dysfunction and disorders.
The Rise of Autoimmune Diseases: The Microbial Deficiency Connection
The dramatic decline in microbial exposure is not only linked to allergies but also autoimmune diseases. For example, in countries where parasitic diseases like malaria are common, there is a lower incidence of rheumatoid arthritis. The reason? The immune system is constantly engaged in battling parasites, preventing it from turning against the body’s own tissues.
Similarly, conditions like multiple sclerosis (MS) and Crohn’s disease have shown an increase in developed countries, where microbial exposure is lower. Studies have shown that people from rural areas with greater microbial exposure (like farmers) are less likely to develop allergies compared to those living in more sanitized urban environments.
The Hygiene Hypothesis in Action:
The hygiene hypothesis proposes that the “sterile” environment in developed nations, free from many infections and parasites, leads to an immune system that is not sufficiently trained. The body may then start to react aggressively to harmless substances like pollen, food, or even its own tissues.
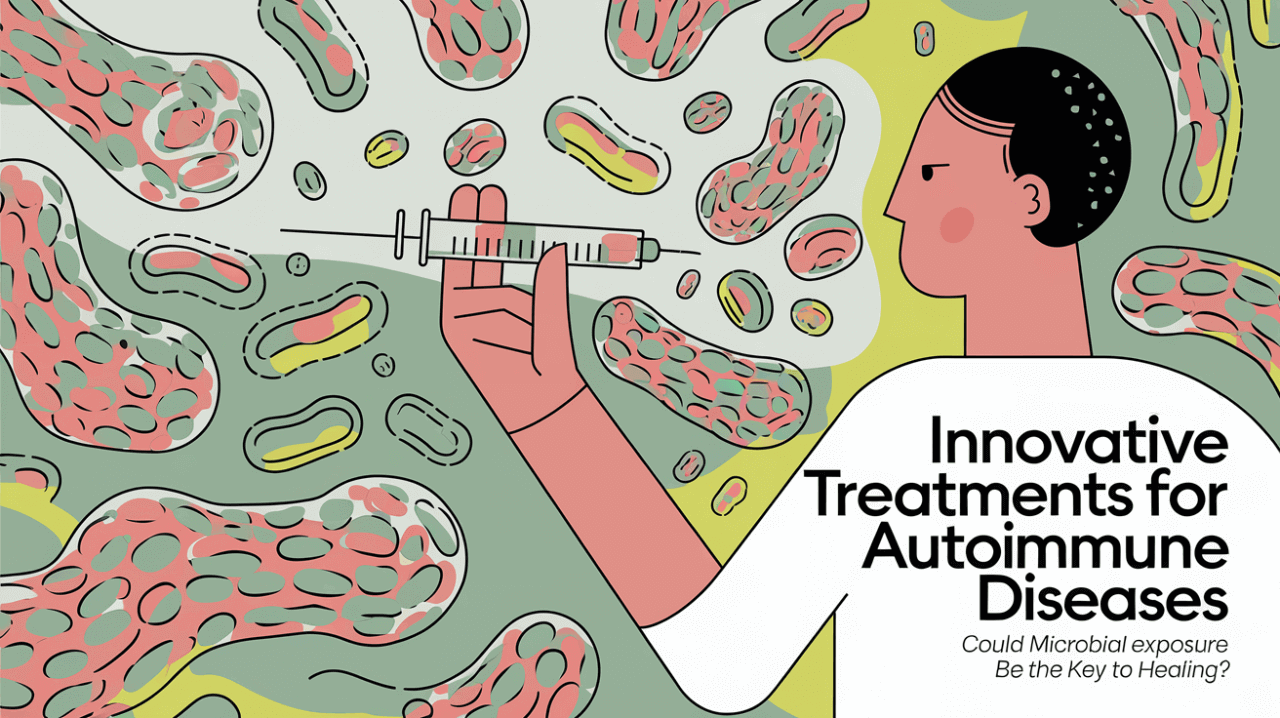
Potential Solutions: Reintroducing Microbes to Balance the Immune System
Therapies Based on Microbial Exposure:
One potential solution to reversing the trend of rising allergies and autoimmune diseases lies in reintroducing microbial exposure. Scientists are exploring therapies that deliberately expose individuals to certain microbes or parasites to help “reset” the immune system. For example, Velasquez-Manoff himself participated in an experimental treatment using the Trichuris trichiura worm, which resulted in improvements in his asthma, allergies, and skin conditions.
Other therapies, like fecal microbiota transplants (FMT), have been tested to restore a healthy balance of gut microbes. Early results suggest that rebalancing the microbiome can have significant health benefits, not only for digestive health but also for the immune system.
Helicobacter Pylori and Its Role:
Another fascinating example is Helicobacter pylori, a bacterium commonly found in the stomach. Historically, H. pylori played a role in modulating the immune system, but as hygiene standards improved, its prevalence decreased. Some researchers now suggest that the absence of H. pylori may contribute to the rise of autoimmune conditions like rheumatoid arthritis and lupus.
Conclusion: The Microbial Balance for Health
Moises Velasquez-Manoff’s An Epidemic of Absence presents a thought-provoking argument about the relationship between microbes, our immune system, and the rising incidence of allergies and autoimmune diseases. The rapid advancements in hygiene and medicine have undoubtedly saved lives, but they have also created an environment where our immune systems are no longer challenged in the same way.
The key challenge moving forward is finding a balance—maintaining sufficient exposure to beneficial microbes while protecting ourselves from harmful pathogens. Whether through innovative therapies or a shift in our lifestyle, the future may offer new ways to restore this balance and reduce the burden of immune system disorders.
For more insights on groundbreaking scientific literature, be sure to visit TalkTheBook.com for weekly reviews and updates.